Burnout: Many Hats and the Dehumanized Doctor
It’s true: doctors don’t like to talk about burnout. It doesn’t put us in a good light but, more pertinent to the recent cautious conversations, it doesn’t feel very safe. No issue that could ever result in punitive action or physician health program intervention for doctors will feel quite safe to us for self-disclosure. Burnout has been grouped in with other issues in a way that invokes the monolith of patient safety and, yet, in direct opposition to what is best for patients, slams the door shut on open authentic dialogue. (1.) This is the wrong route for the conversation to go. Burnout is about systems. It has to start with conversations about systems that deal in blame and shame proliferating and strangulating conversations. It has to address how doctors being human became so difficult to discuss. Doctors have, understandably, been willing to publicly admit what amounts to the tip of the iceberg of the personal ramifications of these systems problems and, sadly, many groups have a vested interest in the status quo.
Unsurprisingly, though, the AMA reported burnout was the most discussed topic of 2015. (2.) Some of those discussions, apart from a few articles in medical journals and mainstream press, were anonymous blogs, or conducted by parties using pseudonyms on social media because that’s how doctors have adapted to talking about the unspeakable things now. Many of the people who write openly have retired from clinical medicine, or are now engaged in wellness programs to help physicians become more resilient. One recent columnist on the KevinMD.com blog reported that no one interviewed on burnout agreed to speak publicly on it. (3.)
While there are some innovative programs, the evidence is still out on the resilience agenda. Most of us started out enormously resilient. I think some of that dialogue can be distracting, and that first, the root causes of burnout should be studied and addressed. There is no doubt that work-life balance is accelerating in the wrong direction and this is part of the problem. The fundamental reasons why that is happening need to be understood. That cannot happen without more studies and more people speaking up using their names.
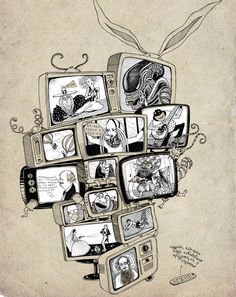
Early in my career, at one point I was asked to take on more responsibility at a difficult clinical job. What had actually happened was that, because someone had been let go, I was being asked informally to take on a second job with no title and ill-defined boundaries. The administrator said to me, as though it were a compliment or a promotion “we all wear many hats.” At the time I didn’t understand this fully. I now see that he was essentially saying- your job is about to get a lot harder as you take on more roles- because these responsibilities are not all compatible.
Having had to write a sort of informal bio recently, I thought briefly of what I would have liked it to say. I imagined briefly being able to write simply something like: doctor, healer, psychotherapist, thinker, writer, human, woman.
And then for a week or so, I reflected on what I actually do with my time. As incredibly fortunate as I am to be still self-employed in name, I see this is a sad list of the many hats that conflict and compete fiercely for resources, colliding constantly in my time. I owe here an acknowledgement to the blog of Dr. Rocky Bilhartz, who unforgettably describes printing a boarding pass in his office first so he can send his patient who is having a heart attack to the hospital. He manages to write about things like this and be funny. (4) That is one very important way we give ourselves permission to write this stuff. It’s tough to do though.
So my informal bio is actually something like this:
Part 1
Prescription writer and refiller
Data entry clerk, document generator, signer, sender, recipient and safekeeper
Medical coder and biller
IT researcher, purchaser, installer, implementer, beta tester and struggling troubleshooter
Pharmacy liaison and support
Prior authorization technician
Purchaser, consumer and examinee of the maintenance of certification medical industrial complex
Regulatory compliance and opportunity cost manager/ Resistant employee
Expectation/Disappointment manager and educator
Unrepentant multitasker/Mindfulness apologist
And with what’s left:
Part 2
Psychiatrist, reader and writer
Privileged grateful witness to stories of people and suffering/Guardian of their privacy
Advocate for the physician-patient relationship
Student of scientific, economic, psychosocial and technological change in medicine and implications
Burnout, as defined by Maslach in 1981, had three fundamental components. She describes depersonalization, emotional exhaustion and diminished sense of personal accomplishment. A big driver I see is the dehumanizing of doctors in medicine. The work itself has devolved as described above. These tasks overwhelm, expand and collide, eclipsing the most important and meaningful work.
The exploding regulatory/punitive climate combined with the digital health revolution is causing a default to our unhealthiest coping. This involves further numbing out and denying our own needs and humanity, until something snaps. The culture has created demoralization, shame and secrecy. We fear retaliation, retribution, being labeled disruptive for being human. There is no way to deal with the repetitive frustrating experiences of eternal unnecessary interruptions, distractions, obstructions and disturbances to the important work- alert fatigue to the brain-other than to just tune some things out. This is inevitably perceived as a kind of callousness, sometimes called compassion fatigue. It is perhaps a mix of emotional exhaustion, depersonalization and survival instincts.
The concept of personal time and space as separate from work has been eroded. Permission, time and space to be human got written out of the blueprint of a profession which requires doctors, in order to be effective, to be acutely and exquisitely human.
The human hat, the one that matters most, doesn’t go so well with the others anymore. I don’t really see many answers yet, as long as we are still not even able to talk openly for fear it could harm our careers or distress patients. The need for anonymity, while freeing many to speak up, is still in the end a symptom of the kind of prison we inhabit where doctors aren’t really allowed to be people.
1.Brown, Goske, Johnson J Am Coll Radiology 2009 July; 6(7):479—85 Beyond substance abuse: stress, burnout and depression as causes of physician impairment and disruptive behavior.
2.AMA Wire Dec 17, 2015
3.Diane W. Shannon, MD Fix the root cause of physician burnout. Not just the symptoms. KevinMD.com blog
4.Bilhartz, Rocky MD Taking Back Medicine blog. “Using Technology to Move Backwards” May 6, 2015